- This information was developed by GMR Web Team.
- This information is intended only to provide general guidance. It does not provide definitive medical advice.
- It is important that you consult your doctor about your specific condition.
Vaginitis
Vaginitis is a common and often uncomfortable gynecological condition characterized by inflammation of the vagina, typically caused by an imbalance of the natural bacterial flora, infections, or irritants. It affects millions of women worldwide, causing symptoms such as itching, burning, abnormal discharge, and discomfort during urination or sexual intercourse. Vaginitis can be caused by various factors, including bacterial vaginosis, yeast infections, trichomoniasis, and atrophic vaginitis, each requiring distinct treatment approaches. If left untreated, vaginitis can lead to complications like increased risk of sexually transmitted infections, pelvic inflammatory disease, and impact on reproductive health.
Understanding the causes, symptoms, and treatment options is essential for effective management and prevention of vaginitis, enabling women to regain comfort, confidence, and optimal vaginal health.
What is Vaginitis?
Vaginitis is a medical condition characterized by inflammation of the vagina, resulting in discomfort, itching, and abnormal discharge. It occurs when the natural balance of bacteria in the vagina is disrupted, leading to an overgrowth of harmful microorganisms or an allergic reaction to irritants. Vaginitis can be caused by various factors, including bacterial vaginosis, yeast infections (candidiasis), trichomoniasis (a sexually transmitted infection), and atrophic vaginitis (thinning of vaginal tissues due to hormonal changes). The condition can affect women of all ages, with symptoms ranging from mild to severe, and if left untreated, can lead to complications such as increased risk of sexually transmitted infections, pelvic inflammatory disease, and impact on reproductive health.
What Are the Types of Vaginitis?
There are several types of vaginitis, including:
- Bacterial Vaginosis (BV): Caused by an overgrowth of harmful bacteria in the vagina.
- Yeast Vaginitis (Candidiasis): Caused by an overgrowth of Candida yeast in the vagina.
- Trichomoniasis: A sexually transmitted infection caused by the Trichomonas vaginalis parasite.
- Atrophic Vaginitis: Thinning and drying of vaginal tissues due to hormonal changes, often during menopause.
- Desquamative Inflammatory Vaginitis (DIV): A rare condition characterized by inflammation and shedding of vaginal tissue.
- Vaginal Atrophy: Thinning and drying of vaginal tissues due to hormonal changes or other factors.
- Allergic Vaginitis: An allergic reaction to irritants such as soaps, spermicides, or latex.
- Irritant Vaginitis: Inflammation caused by exposure to irritating substances.
- Infectious Vaginitis: Vaginitis caused by infections such as herpes, gonorrhea, or chlamydia.
What Causes Vaginitis?
Vaginitis can be caused by a variety of factors, including:
- Bacterial Imbalance: Disruption of the natural balance of bacteria in the vagina, leading to an overgrowth of harmful bacteria.
- Yeast Infections: Overgrowth of Candida yeast in the vagina, often caused by antibiotic use, hormonal changes, or diabetes.
- Sexually Transmitted Infections (STIs): Infections like trichomoniasis, gonorrhea, and chlamydia can cause vaginitis.
- Hormonal Changes: Decreases in estrogen levels during menopause or breastfeeding can lead to atrophic vaginitis.
- Irritants: Exposure to soaps, spermicides, latex, or other substances that can cause allergic reactions or irritation.
- Infections: Bacterial, viral, or fungal infections can cause vaginitis.
- Poor Hygiene: Not practicing good hygiene, such as wiping from front to back, can lead to bacterial transfer and vaginitis.
- Tight-Fitting Clothing: Wearing tight-fitting clothing or synthetic fabrics can trap moisture and create an ideal environment for bacterial growth.
- Douching: Douching can disrupt the natural balance of bacteria in the vagina, leading to vaginitis.
- Medications: Certain medications, such as antibiotics or steroids, can alter the natural balance of bacteria in the vagina.
- Weakened Immune System: Conditions like HIV/AIDS or taking immunosuppressive drugs can increase the risk of vaginitis.
- Pregnancy: Hormonal changes during pregnancy can increase the risk of vaginitis.
- Aging: Thinning and drying of vaginal tissues due to hormonal changes during menopause.
- Surgical Procedures: Certain surgical procedures, such as hysterectomy or radiation therapy, can increase the risk of vaginitis.
What Are the Symptoms of Vaginitis?
The symptoms of vaginitis can vary depending on the type and severity of the condition, but common symptoms include:
- Unusual color, consistency, or amount of discharge may be foul-smelling.
- Vaginal itching, burning, or irritation, which can be severe.
- Inflammation of the vagina and vulva leads to redness and swelling.
- Discomfort or pain while urinating can be a sign of infection.
- Pain or discomfort during sexual intercourse, which can be due to inflammation or dryness.
- Unpleasant or strong vaginal odor, which can be embarrassing.
- Dryness or lack of lubrication in the vagina leads to discomfort or pain.
- Light bleeding or spotting, especially after intercourse.
- General discomfort or feeling of unease in the vaginal area.
- The need to urinate more frequently due to irritation or infection.
How is Vaginitis Diagnosed?
Diagnosing vaginitis involves a combination of the following:
- Medical History: Discussing symptoms, sexual history, and menstrual cycle with a healthcare provider.
- Physical Exam: Visual examination of the vagina and vulva to look for signs of inflammation, discharge, or other abnormalities.
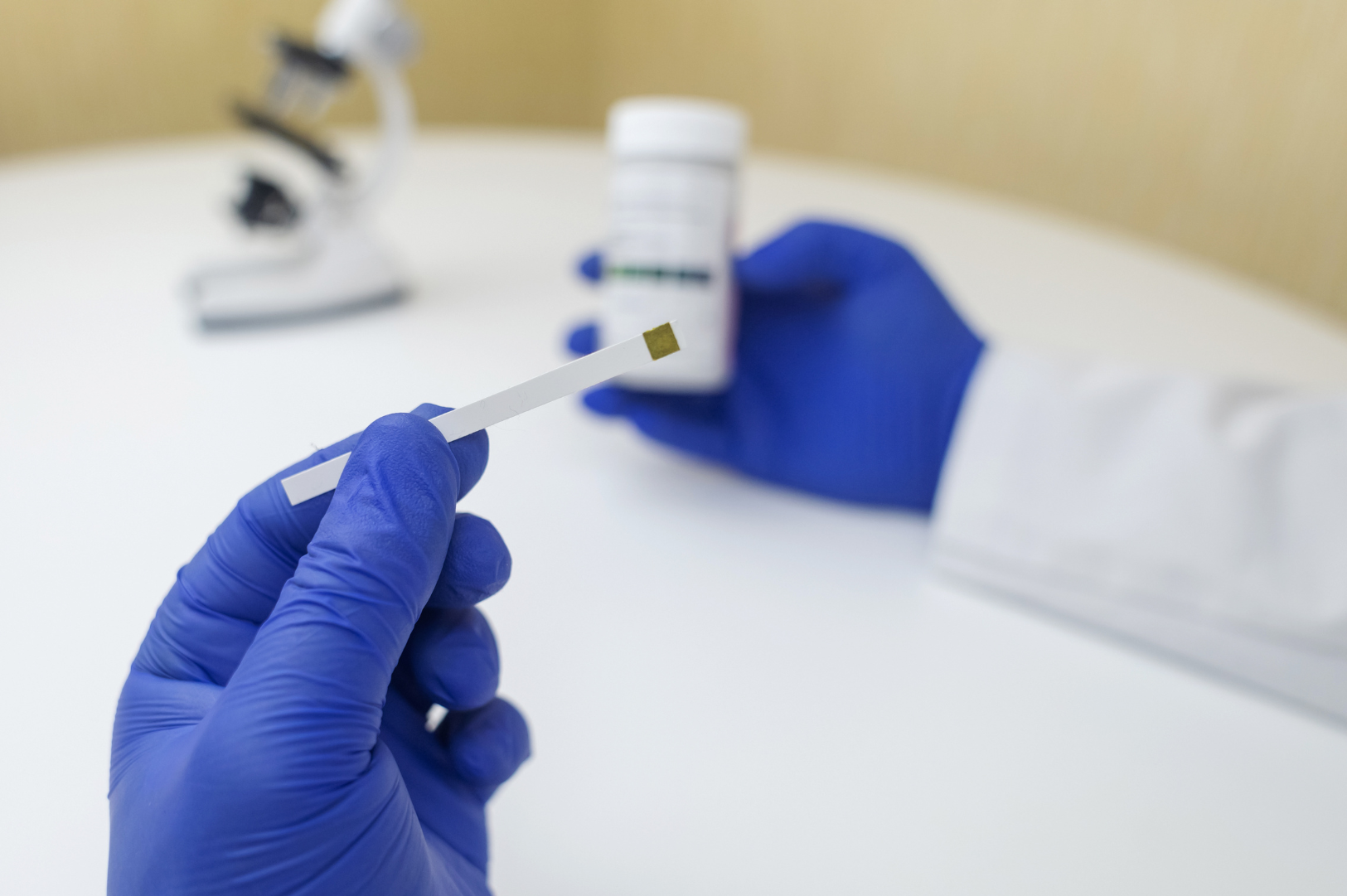
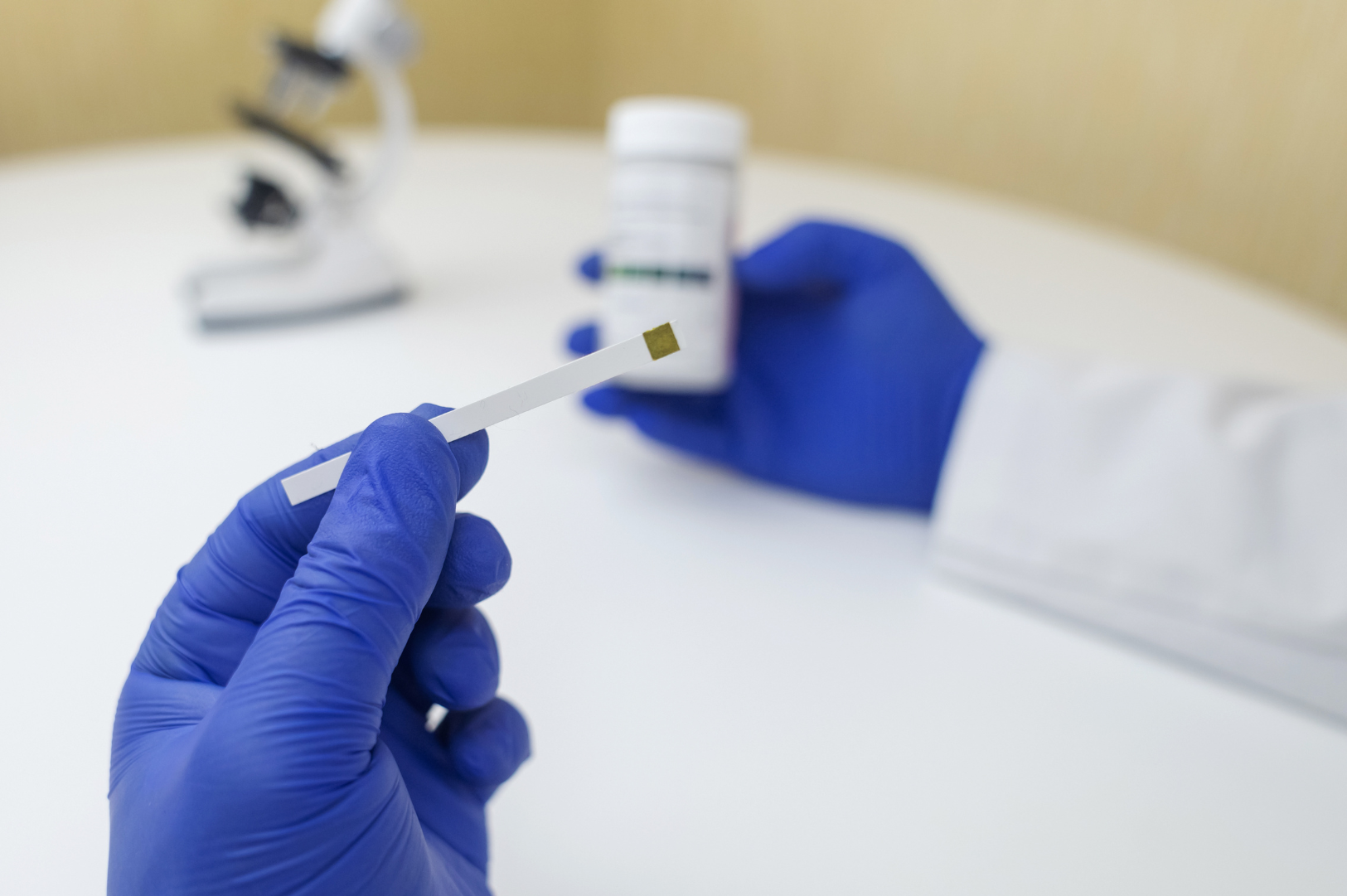
- Vaginal Discharge Examination: Collect a sample of vaginal discharge to examine under a microscope or send it to a laboratory for testing.
- pH Test: Measuring the acidity of the vagina to determine if it's within the normal range.
- Wet Mount: Mixing vaginal discharge with a solution and examining it under a microscope to detect yeast, bacteria, or trichomonads.
- KOH Test: Adding potassium hydroxide to vaginal discharge to detect yeast or other fungal infections.
- DNA Testing: DNA tests detect specific infections like trichomoniasis or gonorrhea.
- Cultures: Taking a sample of vaginal discharge to grow bacteria or yeast in a laboratory to identify the cause.
- Endoscopy: Using a flexible tube with a camera to visually examine the vagina and cervix.
How is Vaginitis Treated?
Treatment for vaginitis depends on the type and severity of the condition, but may include:
- Antibiotics: Oral or topical antibiotics to treat bacterial vaginosis or trichomoniasis.
- Antifungal Medications: Oral or topical antifungal medications to treat yeast infections.
- Anti-itch Creams: Topical creams or ointments to relieve itching and irritation.
- Hormone Replacement Therapy (HRT): For atrophic vaginitis, HRT may be prescribed to restore estrogen levels.
- Vaginal Estrogen Therapy: Localized estrogen therapy to restore vaginal moisture and elasticity.
- Steroid Creams: Topical steroid creams to reduce inflammation and itching.
- Pain Relief Medications: Over-the-counter pain relievers like ibuprofen or acetaminophen to manage discomfort.
- Probiotics: Oral or vaginal probiotics to restore the natural balance of bacteria.
- Home Remedies: Avoiding irritants, practicing good hygiene, and using warm compresses to soothe symptoms.
- Lifestyle Changes: Avoid tight clothing, use breathable fabrics, and avoid scented products.
Can You Prevent Vaginitis?
Here is a concise list of ways to prevent vaginitis:
- Practice good hygiene
- Wear breathable clothing
- Avoid tight-fitting pants
- Use gentle, fragrance-free soap
- Avoid douching
- Wipe from front to back
- Urinate after intercourse
- Use condoms during sex
- Get tested for STIs
- Manage diabetes and HIV (if applicable)
- Avoid scented products
- Use probiotics
- Stay hydrated
- Avoid irritants like latex or spermicides
- Get regular check-ups with a healthcare provider
Takeaway
Vaginitis is a common and treatable condition characterized by inflammation of the vagina, causing discomfort, itching, and abnormal discharge. Bacterial imbalances, yeast infections, STIs, hormonal changes, and irritants can cause it. While symptoms can be uncomfortable, prompt diagnosis and treatment by a healthcare provider can alleviate symptoms and prevent complications. By practicing good hygiene, safe sex, and seeking medical attention when necessary, women can reduce their risk of developing vaginitis and maintain optimal vaginal health.